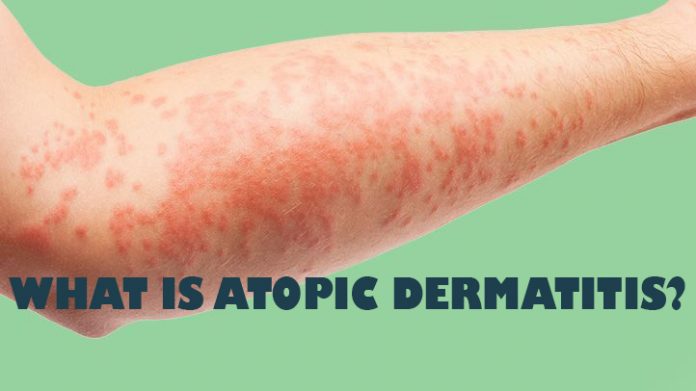
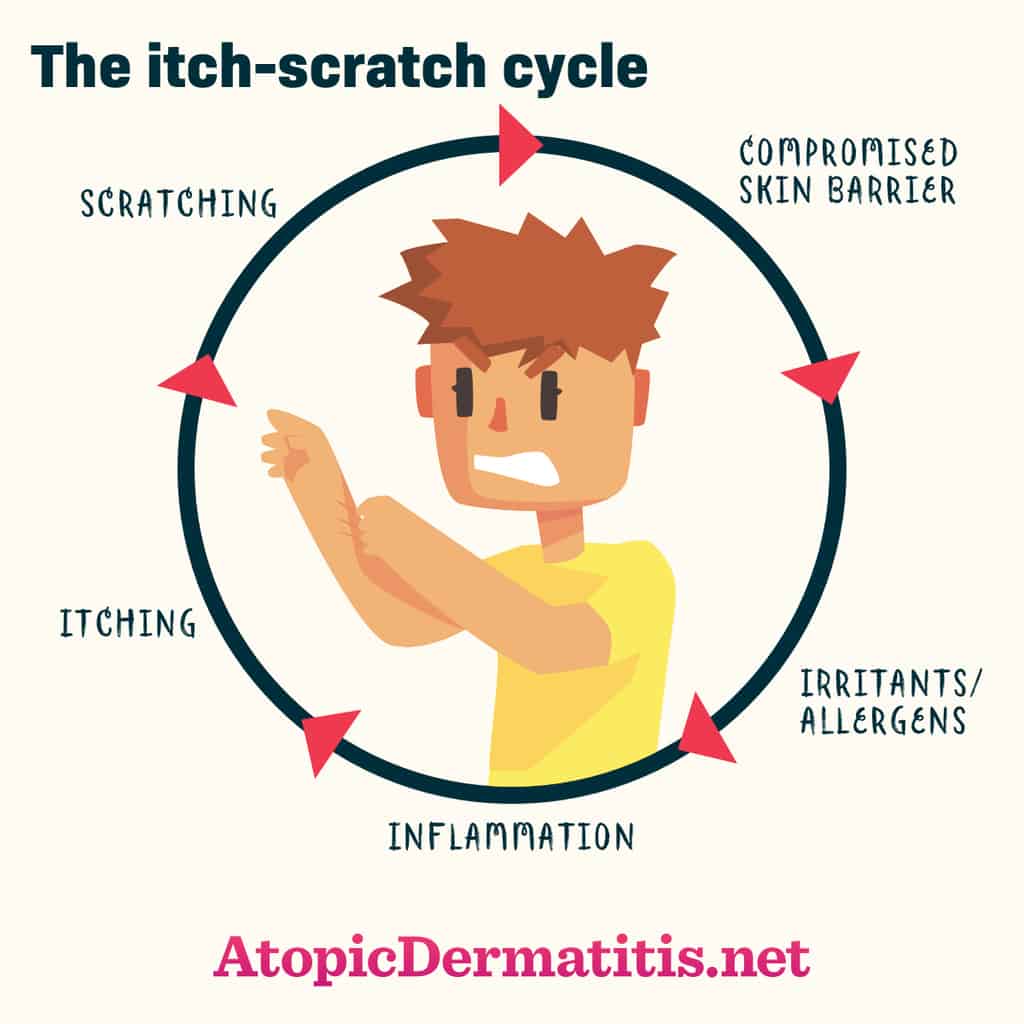
The intense itching in atopic eczema results in an itch scratch cycle which makes the skin thickened or lichenified, a cause for the chronicity of the disease. In most patients there is a family history of eczema, allergic cold (rhinitis) or asthma. 35% of infants affected by atopic dermatitis develop asthma in later life.

Atopic dermatitis develops in the first 2-3 months of life as an acute oozing eczema, starting usually on the cheeks and involving the other body areas later on.
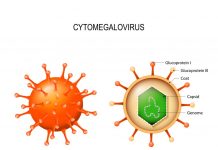
Triggering Factors in Atopic Dermatitis
Triggers of atopic eczema include dust (including pollen and dust mites), bacterial infections, auto- sensitization to human proteins, dry weather, detergents, clothes, stress and, finally certain food items like eggs, milk, peanuts, soybeans, fish, and wheat.
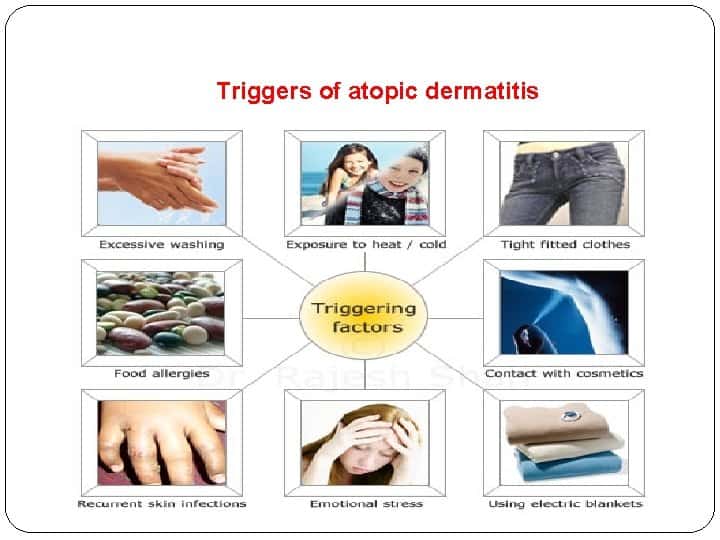
A genetic predisposition is required for these allergens to produce eczema in the infants. There are wide individual variations in responsiveness to the various allergens .
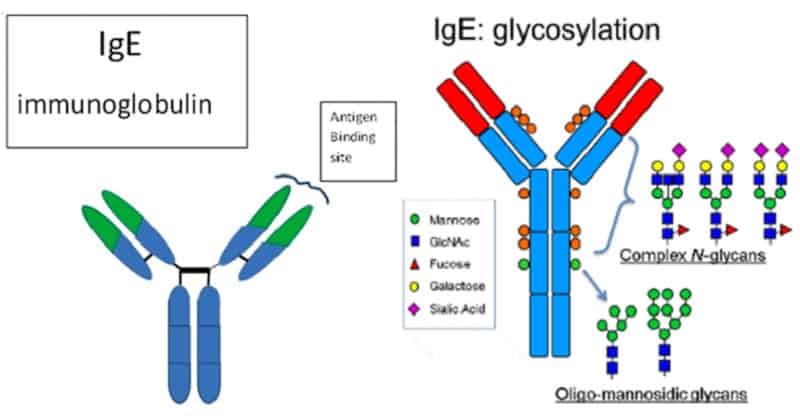
In 85% of affected , the immunoglobulin E (IgE) level is high. IgE is a mediator of allergic skin responses in eczema.
Thus atopic dermatitis is thought to be a result of a complex interaction of compromised skin barrier function, genetic predisposition, environmental, immunological and pharmacological factors in a susceptible individual.
Clinical Features of Atopic Eczema
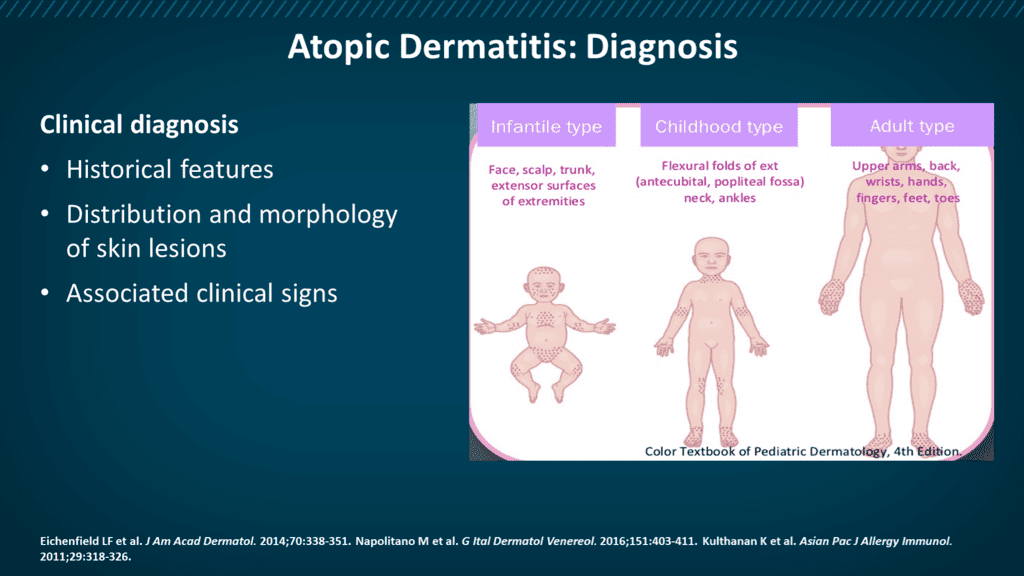
Atopic dermatitis runs a chronic course through infantile, childhood and adult phases.
The patients have dry skin and intense itching.

Indeed, atopic eczema is the itch that rashes! The severe itching leads to constant scratching and rubbing which leads to the skin changes in atopic eczema. This itch scratch cycle, if not controlled, can even have far reaching consequences in the personality development of the child.
In addition to the typical skin changes in various stages of eczema, like acute, sub acute and chronic, the afflicted infant or child may also have seasonal allergic rhinitis (sneezing, running nose, nasal congestion), itching, redness and watering of eyes, throat congestions and, at times, frank asthma.

In acute eczema, the skin is red and puffy, moist and oozing, with erosions and scratch markings. At times there are pus filled blisters and crusts, indicating secondary bacterial infection. In the sub acute stage, the rashes dry up showing crusts and scales on a base of red, inflamed skin.
Repeated scratching and rubbing causes the typical lichenification of the skin with thickening, pigmentation and accentuation of skin marks in chronic, childhood and adult atopic dermatitis.

The common sites affected are the cheeks, forehead, scalp and body in infants, flexural (bending) parts of the arms and legs, wrists, back of hands and feet, eyelids, forehead and generalized in severe cases in the childhood stages. In adult stage, the flexures of the limbs are more often affected, along with neck, elbows and back of the knees.
Diagnosis of Atopic Dermatitis
There are certain diagnostic criteria that dermatologists follow to confirm the diagnosis of atopic dermatitis. Atopic eczema has also got to be differentiated from seborrheic dermatitis, contact dermatitis, psoriasis, early stages of mycosis fungoides and some immunological diseases like Wiskott-Aldrich syndrome, hyper IgE syndrome, Letterer Siwe disease etc.
Laboratory tests include bacterial and viral cultures, IgE studies, skin biopsy etc. The allergy tests rarely help, except in allergies to dust mites, pollens and certain food proteins.
- What Is Aromatherapy Vs. What Are Essential Oils?
- What is La Tomatina in Bunol, Spain Like? What to Expect at the Famous Tomato Throwing Festival
Principles of Management of Atopic Eczema
Education of patient to avoid rubbing and scratching is very important in atopic eczema treatment. The treatment of atopic dermatitis is according to the stage of the disease.

- Atopic dermatitis: Acute eczema treatment.
- Atopic dermatitis: Sub acute eczema treatment.
- Atopic dermatitis: Chronic eczema treatment.
Care should be taken while using topical steroids in infants and children. These should be used only under the supervision of a dermatologist or a pediatrician trained in pediatric dermatology.

Once the inflammation and itching are under control, steroid sparing applications like tar or calcineurin inhibitors like tacrolimus or pimecrolimus cream may be used. The skin should be kept moist with generous use of moisturizing emollients at all times.